Oxygen FAQ
Up to date, expert answers to frequently asked questions (FAQ) about oxygen supply systems, respiratory care and pulse oximetry written by OCC & collaborators.
Maintenance for Oxygen Equipment
- Most are not considered reusable per manufacturer specifications
- Check with the manufacturer specification and clinical guidelines to determine if reuse is safe
- Steps for disinfection must be closely adhered to and may be manufacturer specific
- Some reusable devices (e.g. some ventilator circuits) may have a finite lifespan (e.g. a predefined number of sterilizing cycles)
- Reusability of respiratory care devices is often debated and may vary based on local/national practice guidelines and regulations
Click here to review WHO tips for cleaning and disinfection of respiratory equipment
Additional resources:
- Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care (WHO)
- Disinfectants for COVID-19 (US EPA)
- Cleaning of CPAP and other devices used to administer supplemental oxygen (DPHSS Montana)
- Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. G. Kampf, D. Todt, S. Pfaender, E. Steinmann. Journal of Hospital Infection 104 (2020) 246-251.
- Disinfection and sterilization: an overview. Rutala, Weber. Am J Infect Control
- Disinfectants used for environmental disinfection and new room decontamination technology; Rutala, Weber. Am J Inect Control. 2013
- Guidelines for disinfection and sterilization in healthcare facilities, HICPAC, CDC 2019
- Reuse of anesthesia breathing systems: another difference of opinion and practice between the US and Europe, J Clin Anes 2008
- Bacterial and viral contamination of breathing circuits after extended use – an aspect of patient safety? Acta Anaes Scan, 2016
Solar is a very good power option. PV = photovoltaic – refers to the parameters by which solar panels harness electricity. Electricity is a major cost in PSA systems, so if it’s free, oxygen is essentially free. However, there are so many factors involved in solar design: latitude, how much sun you have, irradiance, cloud cover – it’s hard to generalize. In many parts of the world, including India and much of Africa, we see solar systems with batteries that have a 3-year payback. Problem is lack of funding.
Some of the challenges/considerations that need to be made when using solar options include:
Size: You need to know the size needed. E.g., if your generator requires 12 kW, solar should be sized 60kW to take care of the needs of the entire system. Solar power does not work 24 hours, depending on where you are, so you need to consider this.
Area: For a 280 LPM system, electricity requirements are 20 kW, and require 120 kW with solar, and 12000 sq foot area. Managing area is a big challenge. If you can manage to allocate a 6000 square-foot area, you can maybe install solar in this area so that at least 50% of energy will be through solar means. There are also companies that can provide space to help. Electricity boards allow you to generate electricity in one place, and you can manage the electricity where you need it. The availability of this set up varies state by state.
Investment: Solar can be costly, but there are companies in India giving solar with a 15-year contract and fixed unit charges. In Bombay and Delhi – electricity rates average 9-10 rupees per unit, but with solar you can achieve 6, 6.5 rupees/unit – so it’s cheaper.
If you are using solar then it should be 5 times the actual electricity requirement of a generator.
FAQ by Assist International
PSA plants need to be operated and maintained safely just like any other industrial motor and machinery, but they are not inherently explosive or combustible. The electrical system must be installed properly and safely. However, oxygen is an accelerant for combustion (fire). So, if there is an open flame or ignition source, an enriched oxygen atmosphere can highly accelerate fire. If oxygen is being exhausted even around the plant, there should be no ignition sources, no open flame, no smoking, no sparks allowed. If high pressure oxygen cylinders are being filled, there are additional safety considerations. NOTE: Electricity requirements are pertaining to the model and specification of each individual PSA plant, this specification must be provided by the PSA manufacturer.
FAQ by Assist International
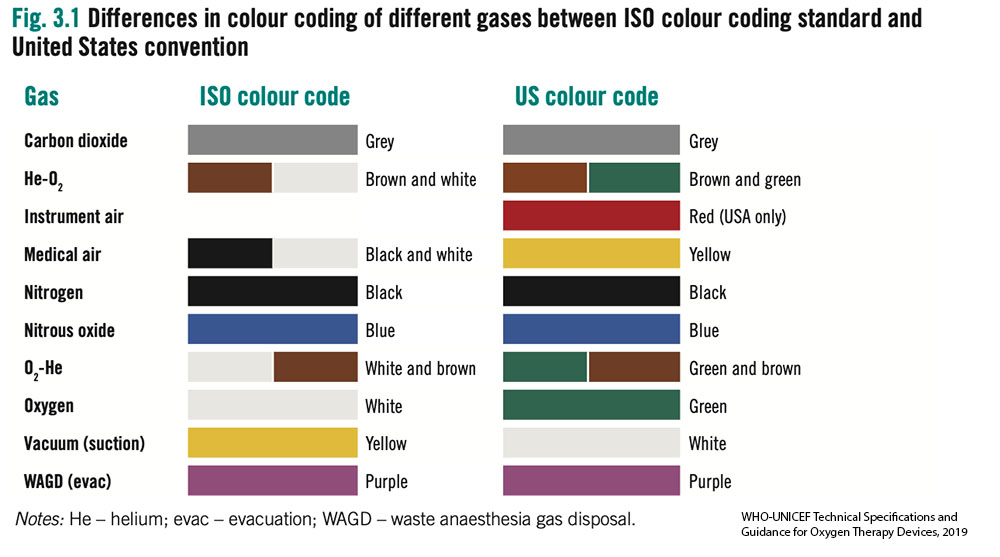
- Without access to an oxygen analyser it can be difficult to determine the gas contents in a cylinder. International standards for color of cylinders are not straightforward.
- Most cylinders are filled using pressure swing adsorption (PSA) oxygen plants and thus have a maximum FiO2 of 95% and often considerably less.
- Older oxygen cylinders may be black with a white top. Outside of these standards many variations also exist. All the cylinders in the images below contained oxygen.
- Oxygen analysers should be used to determine gases before use. Cylinders require routine testing and cleaning by certified technicians. Outlet fittings should be examined for damage or corrosion.

Most oxygen regulators will have a gauge attached, a full J size oxygen cylinder full will have a weight of 78kg (172lb) the oxygen contained in the cylinder weighs approximately 9kg (20)lb, Therefore gauging the volume of oxygen in a cylinder is difficult.

Replace bacterial/viral filters as frequently as supplies allow in accordance with the manufacturer’s recommendations. This recommendation may be as often as every 24 hours, though the optimal interval may differ by setting and determined by assessing the risk:benefit of circuit disconnects, availability of supplies and ability to monitor for malfunctioning filters. Depending on location of the filter placement, circuit setup, humidification system and patient factors, B/V filters may function for multiple weeks, though this would be ‘off-label’ use. If an HME is used, a viral filter can be changed only with signs of increased resistance and may last a week or more. If a heated humidifier is used, the filter in the expiratory limb should be evaluated every 24 hours for signs of increased resistance and may need to be replaced every couple days, although this interval is highly variable. Always refer to the manufacturer’s recommendation. Lifespan may be significantly shortened if nebulized medications are being utilized or if copious secretions are present. Of note, disconnecting circuits can cause risk of aerosolization to healthcare workers.
Passive systems using Heat and Moisture Exchangers (HME) trap moisture and prevent it from being lost from the patient.
- Efficacy of these devices drop over time, causing increased resistance. Manufacturers may suggest a change every 24 hours, but studies have shown that an unsoiled device in some circumstances be used for several days or up to 1 week (Ricard et al, AJRCCM 2000; Thomacot et al, CCM, 2002; AARC. Resp Care. 2012).
- Signs of an increase in resistance include an increase in PIP but no change in Plateau pressure or a prolonged expiratory flow time.
- The most common cause of HME partial occlusion or rise in resistance is from pulmonary edema fluid or blood. Mucus generally clumps in a dependent portion of the device without increasing resistance appreciably. (Davis et al Crit Care Med. 2000)
- Always see manufacturer’s specifications.
- All external filters should be inspected at least daily
- For turbine and compressor ventilators, external inlet filters and fan filters must be cleaned (if cleanable per manufacturer) or replaced at least monthly. For ventilators that allow, bacterial/viral filters should be placed proximal to external inlet filters.
- For example, the LTV-1200: The external inlet filter should be removed and cleaned once a month and can be reused. If operated in high dust or humidity environments, it may need to be cleaned more often. The filter can be cleaned with mild detergent and warm water by using a soft cleaning brush. The filter must be rinsed thoroughly of all detergent residue and must be dried completely prior to re-insertion. If the filter is damaged or cannot be thoroughly cleaned, it should be replaced. The external inlet filter appears to be a proprietary item (Reticulated Foam P/N 10258)
- The fan filter should be removed and cleaned at least once a month (same cleaning procedure as described for the inlet filter). It also can be reused. If the ventilator is being operated in high dust or humidity environments, it may need to be cleaned more often. If the filter is damaged or cannot be thoroughly cleaned, it should be replaced.
- The LTV-1200 model also has an oxygen inlet filter that must be inspected and cleaned on a regular basis. It also is cleaned using a mild cleanser, warm water and a soft brush. Rinse the filter thoroughly to remove all traces of the cleanser. Allow the filter to dry completely before replacing it in the ventilator. Inspect the filter for damage. If it is not intact, or shows signs of damage or cannot be completely cleaned, it should be replaced. The filter is a proprietary item (O2 Inlet Filter (P/N 19845-001) and the accompanying O-Ring (P/N10609)
- The Zoll 731 ventilator: has an internal 2-stage filtration system (an outer foam filter and inner disk filter) to protect the gas flow. External filters should be visually inspected on a daily basis (or more frequently) for dust build up during extended operation in harsh environments and changed when they appear dirty. Use of external filters will preserve the life of the proprietary internal filters (foam filter REF#: 465-0028-00, Air Intake Disk Filter (REF # 465-0027-00). If external filters are not (or cannot be) used, the internal filters must be visually inspected on a regular basis and replaced when dirty. Note: proprietary internal filters cannot be cleaned and reused: they must be replaced.
- The Medtronic PB560 has an external air inlet filter that is intended to be replaced (~monthly or more often) rather than reused
Always reference the manufacturer’s recommendations as this varies. Most vents require a self test upon startup or when used on a new patient. There is additional preventive maintenance at regular scheduled intervals. All external filters should be inspected at least daily and for turbine and compressor ventilators, external inlet filters and fan filters must be cleaned at least monthly.
The primary consideration should be to ensure that the oxygen system is dependable and sustainable. The best main supply source of oxygen to a patient is a direct piped system that connects to the patient bedside from a PSA plant (or oxygen reservoir supplied by a liquid oxygen source). The direct pipe system is highly recommended and preferred. The alternative is to bring cylinders to the bedside. The back-up supply source for a direct pipe system would be a manifold of cylinders and additional spare cylinders to adequately supply the pipe system if the main supply is temporarily not operating.
FAQ by Assist International
There could be many reasons for this. If it is connected to the pipe network, it is possible the design of the pipe was not done correctly. Under “Supplementary Resources”, there are recommendations posted about rational use of oxygen that can provide further detail.
FAQ by Assist International
It depends on many local factors. Consider the materials used locally, how dusty the area is, and how hot the area is. Generally, we prefer to use masonry block and concrete for the walls and concrete floor. For the roof, consider factors such as tropical storm frequency in the area. If the area is subject to tropical storms with high winds, then consider a concrete roof. Also consider thermal mass and/or insulation of roof to minimize heat transmission.
PSA plants are much more expensive if provided in a container (also the time to build is longer). The advantage is ease of installation without a building, but a support building will be needed to manage cylinders that are being filled and the manifold for the cylinder supply (primary supply or backup supply) to a pipe system.
FAQ by Assist International
Key points for sustainability of an oxygen supply system begin with identification of a cost analysis for operational expenses:
- Cost of power to operate 24/7 – include cost of grid power and diesel fuel for back-up generators.
- Cost of spare parts package that is specific for the type of equipment to be installed. For example: key equipment for spare parts includes the air compressor, PSA generator and the booster compressor for filling cylinders (if filling cylinders). Budget for the spare parts and confirm the supply chain to order and import the spare parts.
- Staffing costs of Engineers for service and daily operations.
- Cost of service contracts for outside service provider to do regular maintenance
FAQ by Assist International
Here are some tips on how to safely conserve oxygen depending on the local context:
- Be cautious with high flow nasal cannula – high flow nasal cannula uses up to 60-70 LPM flow and can deplete stores quickly. This delivery device generally should not be used on cylinders unless a manifold system is present and a large cylinder pool is present. Additionally, even when supply may be ample, multiple HFNC devices in simultaneous use may cause system pressure failure or a rate of decline that causes excess freezing of liquid oxygen sources (which will decrease liquid oxygen output further). Always wean patient flows as quickly as possible and transition to alternative lower flow devices as soon as tolerated. There are some turbine and Venturi based devices which do not require a robust medical air supply, but these devices still consume O2 at high rates.
- Use evidence based SpO2 goals and avoid hyperoxia – Avoiding higher than necessary SpO2 goals will save vast quantities of oxygen (Read more on Optimal SpO2 Goals). The difference in SpO2 goal of 90 vs 92% in COVID19 patients can translate to 2-3x less oxygen utilized. This requires continuous or frequent pulse oximetry checks and careful, frequent titration. (see SpO2 goals). There are multiple auto-titration devices that are receiving increasing attention, but yet to see widespread use.
- Consider oxygen conserving devices – There are multiple types of oxygen conserving devices, which may or may not be useful depending on the use case. These devices include oxymizers (both pendant style and nasal reservoir style) as well as conserving devices that are placed on the cylinder directly (also known as ‘pulse dose’ devices). Reservoir-based devices conserve oxygen by enabling a higher FiO2 with lower flow rate as the patient is breathing some oxygen from the reservoir. These devices were designed to work in patients with chronic lung conditions, and their performance in patients with acute respiratory failure is largely unproven (i.e. if a patient has a higher minute ventilation). Pulse dose devices can be expensive. There are numerous other oxygen delivery devices that claim or prove oxygen conservation, however, for most of these devices performance and outcome data are lacking for acute respiratory failure patients.
- Consider liquid oxygen when possible – this is the most efficient way to store and produce oxygen, based on size:capacity. However, liquid oxygen requires considerable infrastructure on site and regionally(e.g. roads, trucks, oxygen separating plants, etc).
- Utilize additional O2 storage methods – these may be mobile liquid oxygen units, additional cylinders (Size H/J), or reservoir devices.
- Inspect and eliminate O2 system leaks – leaks in oxygen infrastructure and delivery devices are common. Common causes to include:
- Using excess flow
- Not turning off devices that not in use (e.g. anesthesia machines or flowmeters)
- Incorrectly secured fitting from cylinders
- Leaks in high or low pressure tubing due to lack of adequate maintenance
- Utilize oxygen concentrators – Consider utilizing oxygen concentrators to preserve cylinders and central supply when possible. There are multiple ways to split an oxygen concentrator to maximize the benefit of its output for multiple patients.
- Carefully adjust intentional leak for CPAP/NIPPV – properly used NIPPV/CPAP will have a leak. Too much or too little can be problematic depending on the interface and patient. Proper titration requires close monitoring and regular adjustment
- Account for Bias Flow & consider devices without bias flow – Some ventilators utilize continuous flow during the expiratory cycle – ‘bias flow.’ In some cases, this adds considerably to oxygen consumption (see ventilator settings in step 3 of this calculator) above and beyond minute ventilation consumption. See manufacturer specifications and account for this in planning.
- Consider systems that allow on-site filling of cylinder – PSA plants and deployable oxygen concentrator systems (DOCS) can be used to refill cylinders. Specifications vary widely depending on need.
- Frequent inspection and countermeasures to avoid liquid oxygen failure:
- Daily inspection to look for excess icing with increased use and colder weather, liquid oxygen evaporators may freeze – dramatically reducing O2 output. Regular inspection and countermeasures are critical (e.g. de-icing or warming systems to prevent freezing
- Inspect daily for potential leaks
- Maintain daily line pressure log and fill level
- Frequent inspection and countermeasures to avoid portable oxygen concentrator failure:
- Avoid running beyond max flow (this can cause humidity to build up in the zeolite and cause decreased efficiency and failure)
- Inspect and clean air intake filter regularly (weekly)
- Ensure functioning voltage stabilization unit if applicable
- Even when not in use, be sure to periodically turn on the concentrator for 30 minutes weekly – this will flush the system and filters of humidity which can damage the device
- Never run the unit without proper filters in place
- Keep the air intake away from walls and curtains
- Frequent inspection and countermeasures to avoid cylinder failure:
- Keep regulators and valves dust free
- Avoid (fire) ignition sources
- Ensure cylinders are stored and secured properly to prevent falling over
- Always open cylinder valves slowly
- Estimate your burn rate and plan ahead – in some settings oxygen shortages can be avoided or ameliorated by planning ahead. Keeping track of daily facility consumption and modeling surge scenarios can help with planning for production and maintenance (PSA plans), cylinder numbers needed, refill frequency (liquid oxygen). There are many tools to help with planning. The online interactive tool (below) helps quickly model ward scenarios with varying levels of detail.
- Ensure adequate power and backup power for PSA/concentrators – power failures can be a significant and abrupt cause of oxygen supply failure. If dependent on oxygen concentrators (whether portable or PSA plant), it is imperative to:
- Utilize voltage stabilization units where power supply voltage is variable
- Implement and regularly test backup power supply and/or backup cylinders in the event of power failure
Additional Resources:
Oxygen supply and demand calculator by OpenCriticalCare.org
Blakeman TC, Branson RD. Oxygen supplies in disaster management. Respir Care. 2013 Jan;58(1):173-83.
Compilation of oxygen planning tools and presentations by OpenCriticalCare.org
Frank’s Hospital Workshop Tutorials – Oxygen Concentrators – by Frank Weithoner
Oxygen conservation infographic – Branson et al, CHEST, May 2021
The first exhaust system directly exhausts the large compressor. The second exhaust would exhaust the room and make sure the room has good air circulation and the temperature is moderated. Also, sometimes the air dryer needs exhaust.
FAQ by Assist International
For staff qualifications, first determine if the staff is expected to simply operate the plant or if the staff is also expected to provide maintenance-service for the plant.
If the staff is expected to simply operate the plant, then the minimum qualification of the should be 1 staff that is a certified/qualified electrical, mechanical, or biomedical technician, plus if cylinders are to be filled, then add staff of 1 or 2 basic laborers to handle cylinders (the number of added laborers needed will depends on the number of cylinders to manage).
If the staff is expected to perform basic and/or advanced maintenance/service to the PSA plant then a certified electrical, mechanical, or biomedical engineer should be added to the staff.
The total number of staff to be hired should be based on the plan of operational hours of the plant. For example, a PSA plant is typically planned to operate for 24 hours per day, 7 days per week, therefore the total number of staff to be hired should be planned accordingly.
Initial Basic Training for PSA plant technicians and engineers is recommended to begin at the time of plant installation and commissioning by the manufacturer’s installation team. The manufacture should provide complete instruction regarding how to operate the plant, monitor, understand and record the proper performance parameters of the plant, instruction of simple and routine maintenance for the plant according to manufacturer’s specification, basic trouble-shooting, and standard operating procedures for acquiring support for service and maintenance when needed.
Advanced levels of service should only be performed by competent trained engineers and technicians, and this usually means that an “outside” service contract will be required to provide the advance levels of service that will be needed. Overall, the availability of advanced level training for PSA services is scarce and will require the PSA owner to prioritize and finance efforts to locate training opportunities to increase the knowledge, skill and abilities of their own technicians and engineers.
FAQ by Assist International
Elimination of a machine mounted inspiratory filter – If a bacterial viral filter is used between the circuit Wye and the patient, then an additional inspiratory filter between the machine and the inspiratory limb may not be necessary to protect the patient (so long as the machine is kept clean and an airway mounted filter and/or expiratory limb filter is used). That is a big “if,” and the use of an inspiratory limb filter at the circuit takeoff is to eliminate this chance of error.
A single inspiratory filter setup (at the wye) has been suggested as an option in settings of severe shortage. This setup may create potential for error and subsequent contamination of the machine. Additionally, the use of one instead of two filters in series significantly decreased viral filtration efficiency. The impact on risk of viral contamination is unknown.
Expiratory limb filter extended use (i.e. not changing between patients) has been suggested by some as an option if severe shortage is faced and appropriate bacterial viral filter is used at the patient. APSF
Relatively simpler devices (e.g. transport ventilators) ’sense’ oxygen input as the presence of a high pressure inlet gas – but does not measure actual oxygen concentration (FIO2). So long as the input pressure was adequate, many devices could not discern whether the concentration of oxygen input is adequate (i.e. 93-99%).
The more sophisticated and newer ICU ventilators and anesthesia machines have internal O2 analyzers. If these devices are connected to a gas input that is of adequate pressure but low oxygen concentration, they may either alarm or not function properly. The alarm may have to be disabled but this will vary by manufacturer.
In summary, if you connect a source of oxygen with low concentration, some ventilators may have no idea and not alarm, but other ventilators may sense this and not function properly or alarm (which you may or may not be able to disable).