Oxygen FAQ
Up to date, expert answers to frequently asked questions (FAQ) about oxygen supply systems, respiratory care and pulse oximetry written by OCC & collaborators.
Respiratory Care Consumables
- Most are not considered reusable per manufacturer specifications
- Check with the manufacturer specification and clinical guidelines to determine if reuse is safe
- Steps for disinfection must be closely adhered to and may be manufacturer specific
- Some reusable devices (e.g. some ventilator circuits) may have a finite lifespan (e.g. a predefined number of sterilizing cycles)
- Reusability of respiratory care devices is often debated and may vary based on local/national practice guidelines and regulations
Click here to review WHO tips for cleaning and disinfection of respiratory equipment
Additional resources:
- Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care (WHO)
- Disinfectants for COVID-19 (US EPA)
- Cleaning of CPAP and other devices used to administer supplemental oxygen (DPHSS Montana)
- Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. G. Kampf, D. Todt, S. Pfaender, E. Steinmann. Journal of Hospital Infection 104 (2020) 246-251.
- Disinfection and sterilization: an overview. Rutala, Weber. Am J Infect Control
- Disinfectants used for environmental disinfection and new room decontamination technology; Rutala, Weber. Am J Inect Control. 2013
- Guidelines for disinfection and sterilization in healthcare facilities, HICPAC, CDC 2019
- Reuse of anesthesia breathing systems: another difference of opinion and practice between the US and Europe, J Clin Anes 2008
- Bacterial and viral contamination of breathing circuits after extended use – an aspect of patient safety? Acta Anaes Scan, 2016
No. All ventilators have pre specified limits on the size of patient they can safely support. Manufacturers’ information must always be referenced to determine the recommended patient size as well as the necessary components required for such care. Failure to account for this can result in serious harm.
Key considerations:
- Tidal volume limits – The lower limit of patient size is most often determined by the lower limit of tidal volume that the ventilator can accurately deliver. This limit must be referenced from the user’s manual. For example, if the tidal volume lower limit of a ventilator is specified to be 150mL, and you wish to deliver lung protective ventilation (6mL/kg), then the smallest patient that can be supported can way no less than 25kg (150/6=25). Of note, most international standards require delivered tidal volume to be accurate to within +/- 10% of the set value.
- Circuits – The use of ventilators on smaller patients may require smaller circuits (check manufacturer specifications). These circuits have lower compliance, and thus less tidal volume is ‘lost’ to circuit expansion with pressurization. These circuits also have more resistance and less overall weight. Some ventilators will calibrate themselves during self check to account for circuit compliance and ‘compressible volume’ (Note: this calibration only applies during volume control ventilation and cannot be accounted for during pressure control ventilation). Some ventilators are factory calibrated to account for a pre-specified circuit compliance and thus are intended to be used only with certain proprietary circuits. For example, if an adult circuit (compliance 2.5 ml/cmH20) is used on a 10kg child (goal tidal volume 60-80mL), and the ventilator is set to deliver 20 cmH20 inspiratory pressure, then 50mL (2.5 ml/cmH20 x 20 cmH20 = 50mL) of volume can be expected to be ‘lost’ to expansion of the circuit. Depending on the ventilator brand, pre check calibration and mode, this lost volume may not be accounted for and the patient may receive little if any true ventilation.
- Dead Space – special consideration for connectors beyond the patient Wye is always important, but especially essential when managing smaller patients to avoid increasing dead space ventilation.
Below are a few examples of different weight limits for select ventilators:
LTV2/2200
10
50
10 - 20 kg
Zoll 731
5
50
5 - 25 kg
PB 560
5
50
5 - 23 kg
No. There are many different types of ventilator circuits and not all can be used interchangeably. Even for circuits that can functionally be used interchangeably (i.e. they will connect to the ventilator and patient), there may be differences in deadspace and circuit compliance that must be considered. If you would like to learn more, please see question “What different types of ventilator circuit exist?”
The amount of water consumed per day by active humidification depends upon several factors including minute ventilation requirements and the ability of a specific humidification system to reach and maintain the goal of providing between 33 to 44 mgH2O/L of ventilation. Under ideal conditions (use of a heated wire circuit to prevent rainout) at low (5L/min), average for critical-illness (10L/min) and high (15 L/min) minute ventilation demands, the estimated daily consumption would be approximately the following: For the gas conditioning criteria of 33-44 mgH20/L estimated H2O consumption would be approximately 250-300, 500-600 and 700-1000 mL/day, respectively.
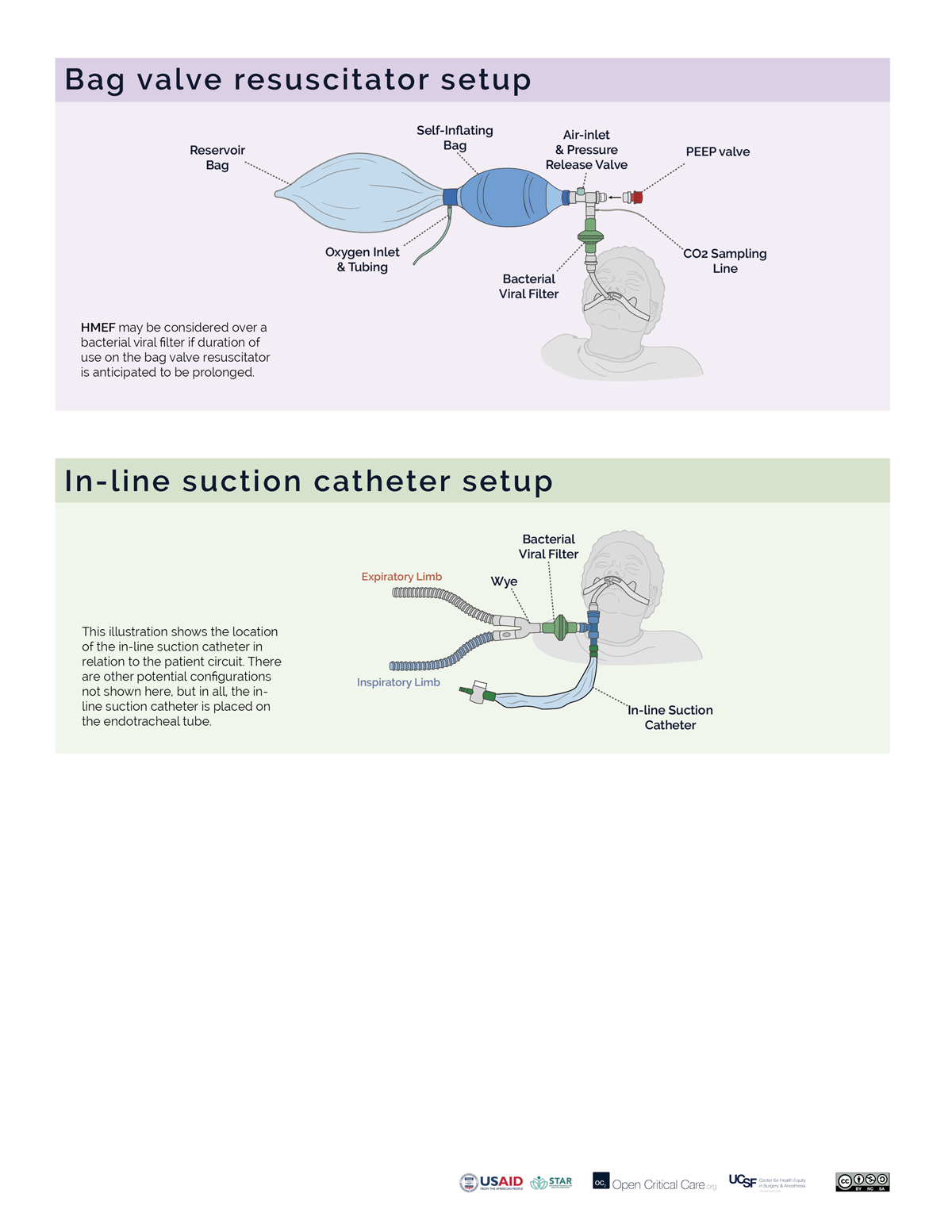
Replace bacterial/viral filters as frequently as supplies allow in accordance with the manufacturer’s recommendations. This recommendation may be as often as every 24 hours, though the optimal interval may differ by setting and determined by assessing the risk:benefit of circuit disconnects, availability of supplies and ability to monitor for malfunctioning filters. Depending on location of the filter placement, circuit setup, humidification system and patient factors, B/V filters may function for multiple weeks, though this would be ‘off-label’ use. If an HME is used, a viral filter can be changed only with signs of increased resistance and may last a week or more. If a heated humidifier is used, the filter in the expiratory limb should be evaluated every 24 hours for signs of increased resistance and may need to be replaced every couple days, although this interval is highly variable. Always refer to the manufacturer’s recommendation. Lifespan may be significantly shortened if nebulized medications are being utilized or if copious secretions are present. Of note, disconnecting circuits can cause risk of aerosolization to healthcare workers.
Passive systems using Heat and Moisture Exchangers (HME) trap moisture and prevent it from being lost from the patient.
- Efficacy of these devices drop over time, causing increased resistance. Manufacturers may suggest a change every 24 hours, but studies have shown that an unsoiled device in some circumstances be used for several days or up to 1 week (Ricard et al, AJRCCM 2000; Thomacot et al, CCM, 2002; AARC. Resp Care. 2012).
- Signs of an increase in resistance include an increase in PIP but no change in Plateau pressure or a prolonged expiratory flow time.
- The most common cause of HME partial occlusion or rise in resistance is from pulmonary edema fluid or blood. Mucus generally clumps in a dependent portion of the device without increasing resistance appreciably. (Davis et al Crit Care Med. 2000)
- Always see manufacturer’s specifications.
- All external filters should be inspected at least daily
- For turbine and compressor ventilators, external inlet filters and fan filters must be cleaned (if cleanable per manufacturer) or replaced at least monthly. For ventilators that allow, bacterial/viral filters should be placed proximal to external inlet filters.
- For example, the LTV-1200: The external inlet filter should be removed and cleaned once a month and can be reused. If operated in high dust or humidity environments, it may need to be cleaned more often. The filter can be cleaned with mild detergent and warm water by using a soft cleaning brush. The filter must be rinsed thoroughly of all detergent residue and must be dried completely prior to re-insertion. If the filter is damaged or cannot be thoroughly cleaned, it should be replaced. The external inlet filter appears to be a proprietary item (Reticulated Foam P/N 10258)
- The fan filter should be removed and cleaned at least once a month (same cleaning procedure as described for the inlet filter). It also can be reused. If the ventilator is being operated in high dust or humidity environments, it may need to be cleaned more often. If the filter is damaged or cannot be thoroughly cleaned, it should be replaced.
- The LTV-1200 model also has an oxygen inlet filter that must be inspected and cleaned on a regular basis. It also is cleaned using a mild cleanser, warm water and a soft brush. Rinse the filter thoroughly to remove all traces of the cleanser. Allow the filter to dry completely before replacing it in the ventilator. Inspect the filter for damage. If it is not intact, or shows signs of damage or cannot be completely cleaned, it should be replaced. The filter is a proprietary item (O2 Inlet Filter (P/N 19845-001) and the accompanying O-Ring (P/N10609)
- The Zoll 731 ventilator: has an internal 2-stage filtration system (an outer foam filter and inner disk filter) to protect the gas flow. External filters should be visually inspected on a daily basis (or more frequently) for dust build up during extended operation in harsh environments and changed when they appear dirty. Use of external filters will preserve the life of the proprietary internal filters (foam filter REF#: 465-0028-00, Air Intake Disk Filter (REF # 465-0027-00). If external filters are not (or cannot be) used, the internal filters must be visually inspected on a regular basis and replaced when dirty. Note: proprietary internal filters cannot be cleaned and reused: they must be replaced.
- The Medtronic PB560 has an external air inlet filter that is intended to be replaced (~monthly or more often) rather than reused
Many would argue that ideally, breathing circuits should be changed between new patients though do not necessarily need to be changed on a routine basis for the same patient; change the breathing circuit only if it has been soiled or damaged (Han, Liu. Respir Care 2010).
However, it is important to note:
- there is considerable practice variation on this (especially prior to the pandemic and especially with anesthesia breathing circuits); often depends on local/national regulations and patient specific factors
- circuit change practices have considerable impact on the environment
Additional Readings:
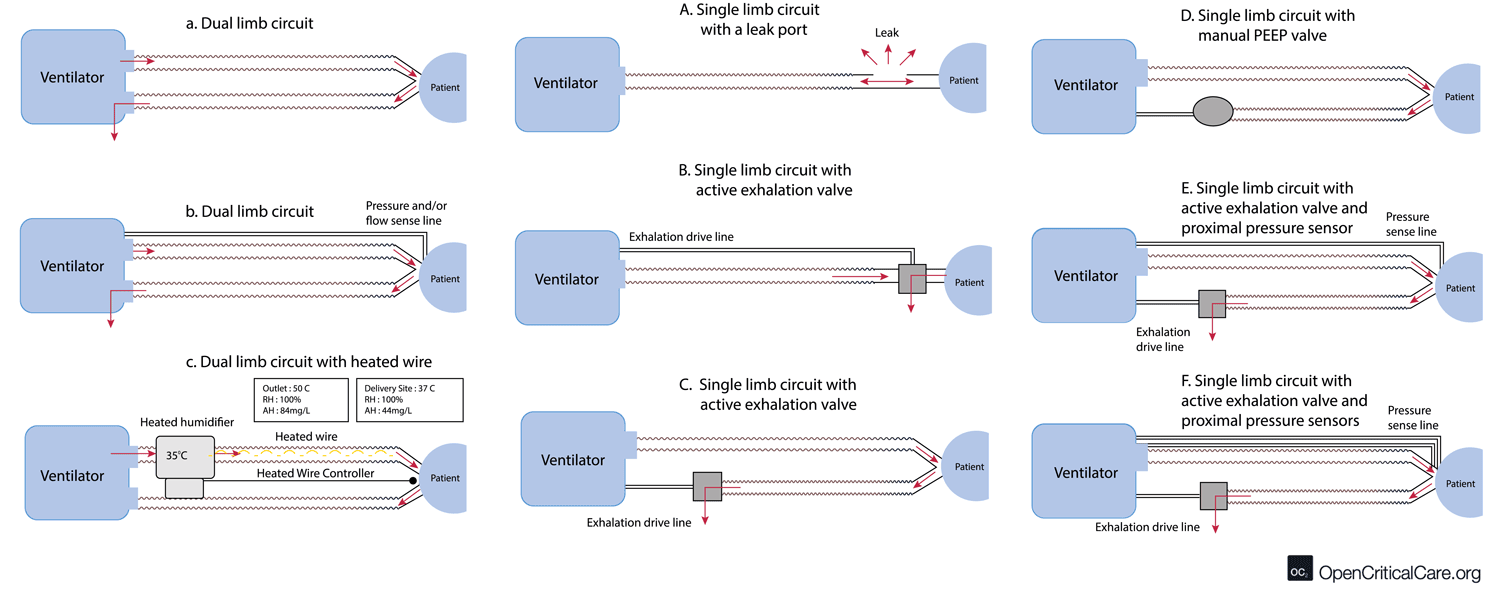
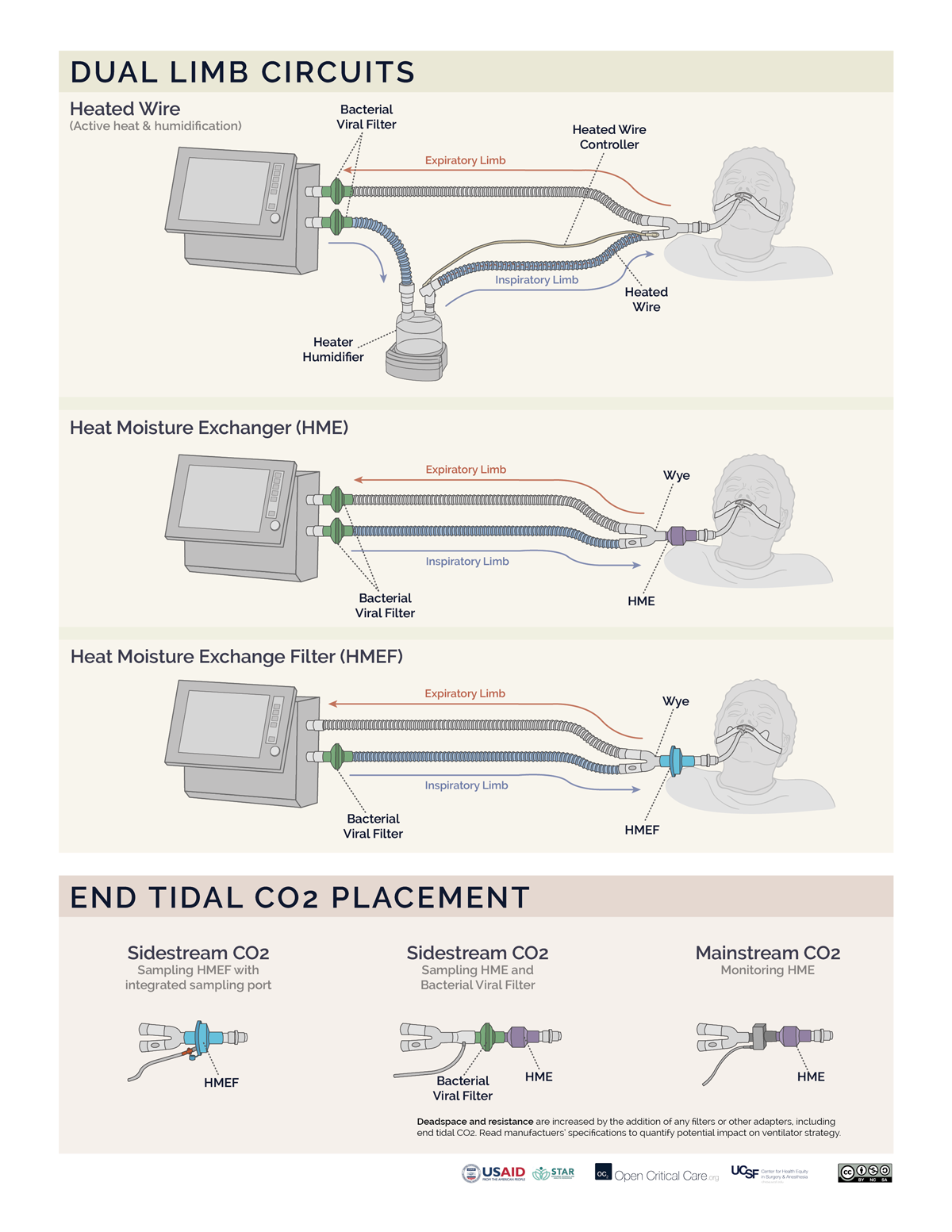
- There are multiple configurations of dual and single limb circuits (outlined below).
- Note on humidification & circuit configuration: some dual and single limb circuits may contain a heated wire in the inspiratory limb to optimize heat & humidification delivery to the patient and to prevent excess condensation from accumulating when using an active heated humidification system. If an active heated humidification system is used in the absence of a heated wire inspiratory limb, a water trap is often needed. Some water traps may allow for emptying without circuit disconnect (an important consideration with COVID19).
- Dual limb circuit (Figure a, b and c) – used by most traditional critical care ventilators. Flow/pressure and PEEP are commonly measured/controlled in the machine, and thus no additional circuit transducer tubing is needed (a). Some circuits do use proximal flow/pressure sensors (b). These may include a heating element in the inspiratory limb and port for temperature monitoring (c).
- Standard single limb with built in leak (figure A) – mostly for non invasive devices
- Standard single limb circuit with active exhalation valve and internal PEEP – (figure B and C) – These circuits are made by multiple manufacturers and can work with multiple vent models.
- Standard single limb circuit with active exhalation valve and manual PEEP – (figure D)
- Standard single limb circuit with active exhalation valve, internal PEEP and proximal pressure sensor – (figure E) – this is one of the most common single limb circuit setups
- Standard single limb circuit with active exhalation valve, internal PEEP and two proximal pressure/flow sensors – (figure F) – this is usually a proprietary circuit type that is commonly encountered and allows measurement of exhaled tidal volume
- It depends on the device setup. Ventilators may require ‘external’ filters (viral, HME, and fan, as well as air intake filters for turbine or compressor ventilators) and internal filters (oxygen inlet filter). Filters can provide three kinds of functions:
-
- Filtering particulate matter
- HEPA (high-efficiency particulate air) filters rated to 3 microns are generally considered ‘acceptable’ for bacterial and viral filtration. The term HEPA refers to the efficiency of capturing particles with a MPPS (most penetrating particle size) diameter of 0.3 microns.
- Of note, machines that accept 50psi/4bar gas intake usually have internal bronze sintered filters to protect the machine from contaminated gas sources. On occasion additional external filters on the high pressure gas lines are required to prevent damage to the device.
- Preserving heat and moisture
- Heat and Moisture Exchangers (HME) are commonly rated to 3 microns, the HEPA standard (and may be referred to as HME filters – HMEF), but may not be. They are composed of foam, paper or other material that allows moisture to condense.
- Hygroscopic Condenser Humidifiers (HCH) are functionally the same as HMEs, though have a slightly different mechanism as they are impregnated with a salt to aid in moisture condenstation. In the past, HME types were separated based on the additional treatment of the media. An HME relied solely on physical principles (the earliest ones were all aluminum) whereas the HCH included treatment of the media with a hygroscopic salt (LiCl, now mostly CaCl). At present, the reality is that most HME devices also take advantage of the hygroscopic salt (check manufacturer’s specifications to confirm this). In theory, if one were to push the media out of an HME then touch it to the tip of the tongue – it would be very salty (DO NOT TRY THIS).
- The moisture efficiency of an HME or HCH is dependent on its size, media density and salt treatment.
- HMEs may be referred to as type I (adult) and type II (pediatrics), which differ in deadspace and functional tidal volume range.
- Unless specifically designated as having capacity for ‘filtration’ (HMEF), HMEs do not provide adequate filtration of bacteria and viruses.
- Filtering bacteria and viruses
- Bacterial/viral (B/V) filters are defined by the ability to filter particles with a diameter size of 3 microns though may be rated to particles as small as 0.2 microns, and do not necessarily provide heat/moisture preservation.
- The minimum viral filtration efficiency (VFE) that is needed to ensure SARS COV-2 virus can not pass from the patient to the room or machine is unknown.
- B/V filters with 99.97% ASTM efficiency or filters with >95% efficiency for MPPS of 0.3 microns may be recommended to prevent SARS-CoV-2 viral transmission though data and standards continue to evolve.
- Diameter for SARS-CoV-2 virion is ~0.06-0.14 microns, hepatitis C is 0.03 microns and Staph aureus is 1 micron.
- Filtering particulate matter
- Combination filters providing all three functions are available. Filters that conserve heat and moisture and provide B/V filtering are often referred to as HMEF.
- More info on filter types and efficiency testing
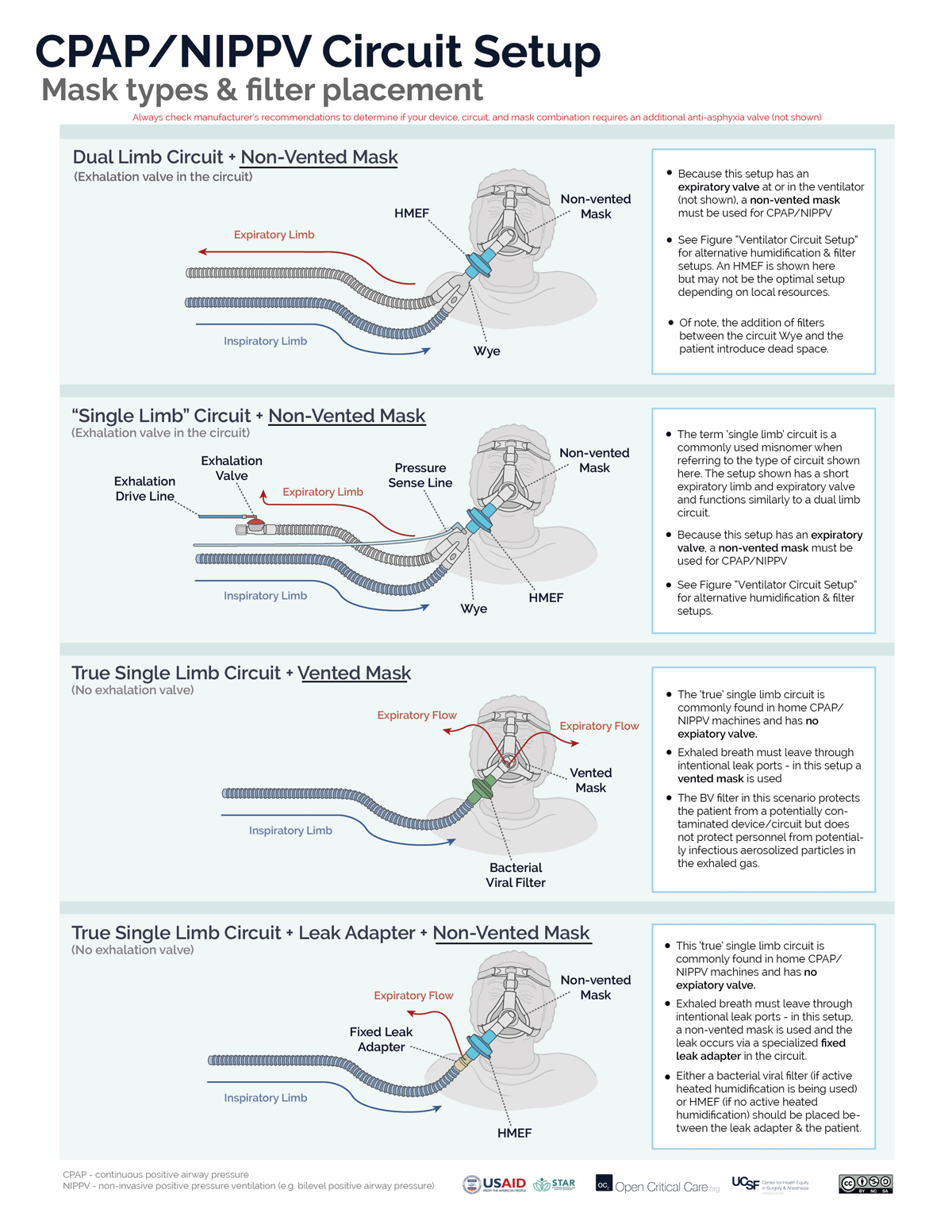
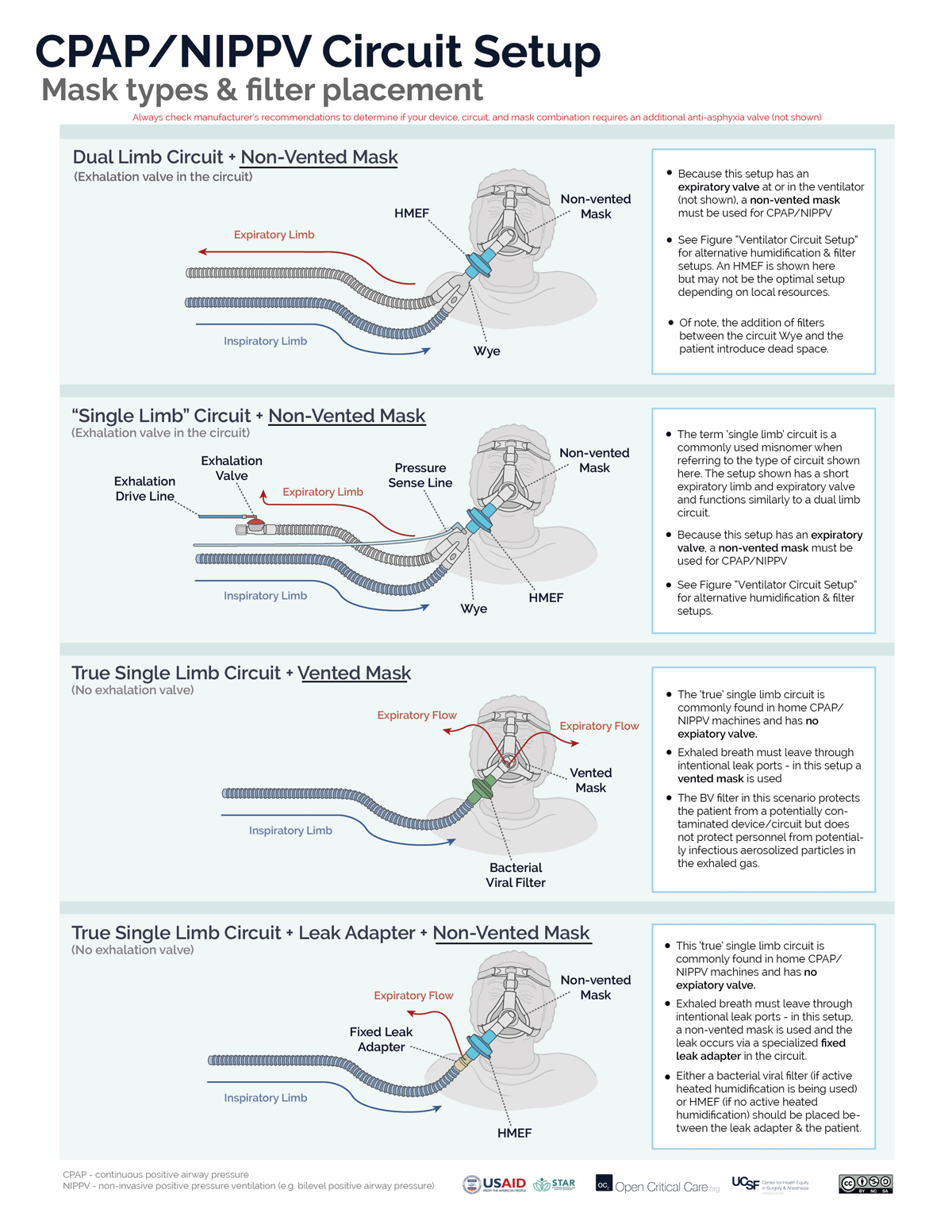
It depends on several factors. Not all masks, circuits or devices are compatible or able to deliver CPAP/NIPPV.
The basis of non-invasive CPAP/NIPPV is a constant gas flow against an expiratory resistor that creates positive “back pressure” in the circuit (i.e. Pressure = Flow x Resistance). Back pressure is increased either by increasing gas flow against the resistor or increasing the resistance to gas flow.
There are 2 circuit options for non-invasive CPAP (or NIPPV/BiPAP):
- A “true” single limb circuit (commonly found in home NIPPV/BiPAP devices) has 1 hose directing gas from the device to the mask and no active expiratory valve. There are two common setups for NIPPV/CPAP with a true single limb circuit. (Note: circuits with both an inspiratory limb and a short expiratory limb with expiratory valve, while commonly referred to as ‘single limb’ are not ‘true’ single limb circuits)
- “Vented Mask” setup – The exhaled breath has to get out of the patient/circuit somewhere, therefore, the mask must act both as the resistor and the exhalation port. A vented mask has holes that allow for fixed resistance. Because the resistance is fixed, CPAP is increased by increasing flow through the circuit.
- Fixed leak valve circuit setup – An alternative option to using a vented mask, is to use a non-vented mask and to place the fixed/intentional leak into the circuit by adding a ‘leak valve,’ which contains holes that allow fixed resistance.
- A dual limb circuit (commonly found in ICU and transport ventilator) has 2 hoses connected by a “Y” (or “wye”) adapter where the expiratory limb directs gas flows to an active expiratory valve that controls expiratory resistance. The expiratory valve either is clearly visible in the expiratory hose (“expiratory manifold”) or the expiratory hose attaches directly back into the ventilator (i.e. the expiratory manifold is built into the ventilator). To function properly (ie to create/adjust CPAP, or pressure-support/ BiPAP) the circuit must only be used with a non-vented mask (i.e. the ventilator will control both gas flow and resistance).
- Troubleshooting Note: Using a vented mask with any dual limb ventilator circuit will result in the inability to effectively create sufficient positive pressure, increased aerosolization and likely set-off alarms.
Some ventilators can utilize both true single limb and dual limb setups. Another approach to determine the correct mask type for NIPPV/CPAP is to determine if the system (ventilator or circuit) has an an active exhalation valve:
- System with active exhalation valve – non-vented mask required
- System without active exhalation valve – vented mask required (or fixed leak adapter in the circuit)
When access to optimal equipment is not readily available, alternative solutions (https://link.springer.com/article/10.1007/s41782-020-00092-7) have been proposed and reported with uncertain outcomes. These are most often not in line with manufacturers’ recommendations and are not endorsed here. Always check manufacturer recommendations for all devices to confirm correct equipment and mode settings.
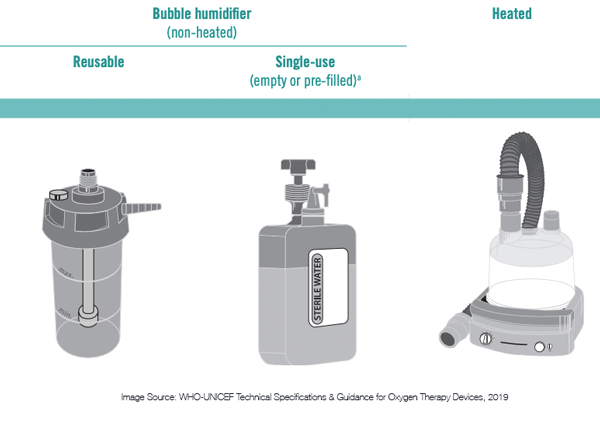
- Passive systems:
- Non-heated bubble humidifiers – are simple, low cost devices used with low flow oxygen delivery devices like nasal cannula or nasopharyngeal catheters. These devices require sterile or distilled water and are generally not efficient. Some may be reusable or single-use only.
- Heat and Moisture Exchangers (HME) are simple, low cost components used with mechanical ventilators and CPAP or NIPPV devices. HMEs trap moisture and prevent it from being lost into the ventilator. They are not reusable.
- Efficacy of these devices drop over time, causing increased resistance. Many manufacturers suggest a change every 24 hours, but studies have shown that an unsoiled device in some circumstances can be used for several days (Ricard et al, AJRCCM 2000; Thomacot et al, CCM, 2002).
- Signs of an increase in resistance include an increase in PIP but no change in Plateau pressure or a prolonged expiratory flow time.
- The most common cause of HME partial occlusion or rise in resistance is from pulmonary edema fluid or blood. Mucus generally clumps in a dependent portion of the device without increasing resistance appreciably. (Davis et al Crit Care Med. 2000)
- Read more about how often HMEs should be replaced
- Hygroscopic Condenser Humidifiers (HCH) are functionally the same as HMEs (though have a slightly different mechanism). In the past, HME types were separated based on the additional treatment of the media. An HME relied solely on physical principles whereas the HCH included treatment of the media with a hygroscopic salt (LiCl, now mostly CaCl). An HME may be made from foam, paper or other substance that helps water condense (the earliest were aluminum). At present, the reality is that most HME devices also take advantage of the hygroscopic salt (check manufacturer’s specifications to confirm this). In theory, if one were to push the media out of an HME then touch it to the tip of the tongue – it would be very salty (DO NOT TRY THIS). The moisture efficiency of an HME or HCH is dependent on its size, media density and salt treatment. HMEs may be referred to as type I (adult) and type II (pediatrics), which differ in deadspace and functional tidal volume range.
- Active systems:
- Active heated humidification systems use a reservoir of water and a heating element. Inhaled air is typically passed through this heated chamber to become humidified before it enters the patient. Ideally, the inspiratory limb of the circuit contains a heating element to preserve the heat and humidification and to keep excess water from condensing and pooling in the circuit.
- These systems require power, a supply chain for sterile or distilled water, and additional disposable tubing.
- Active heated humidification systems use a reservoir of water and a heating element. Inhaled air is typically passed through this heated chamber to become humidified before it enters the patient. Ideally, the inspiratory limb of the circuit contains a heating element to preserve the heat and humidification and to keep excess water from condensing and pooling in the circuit.
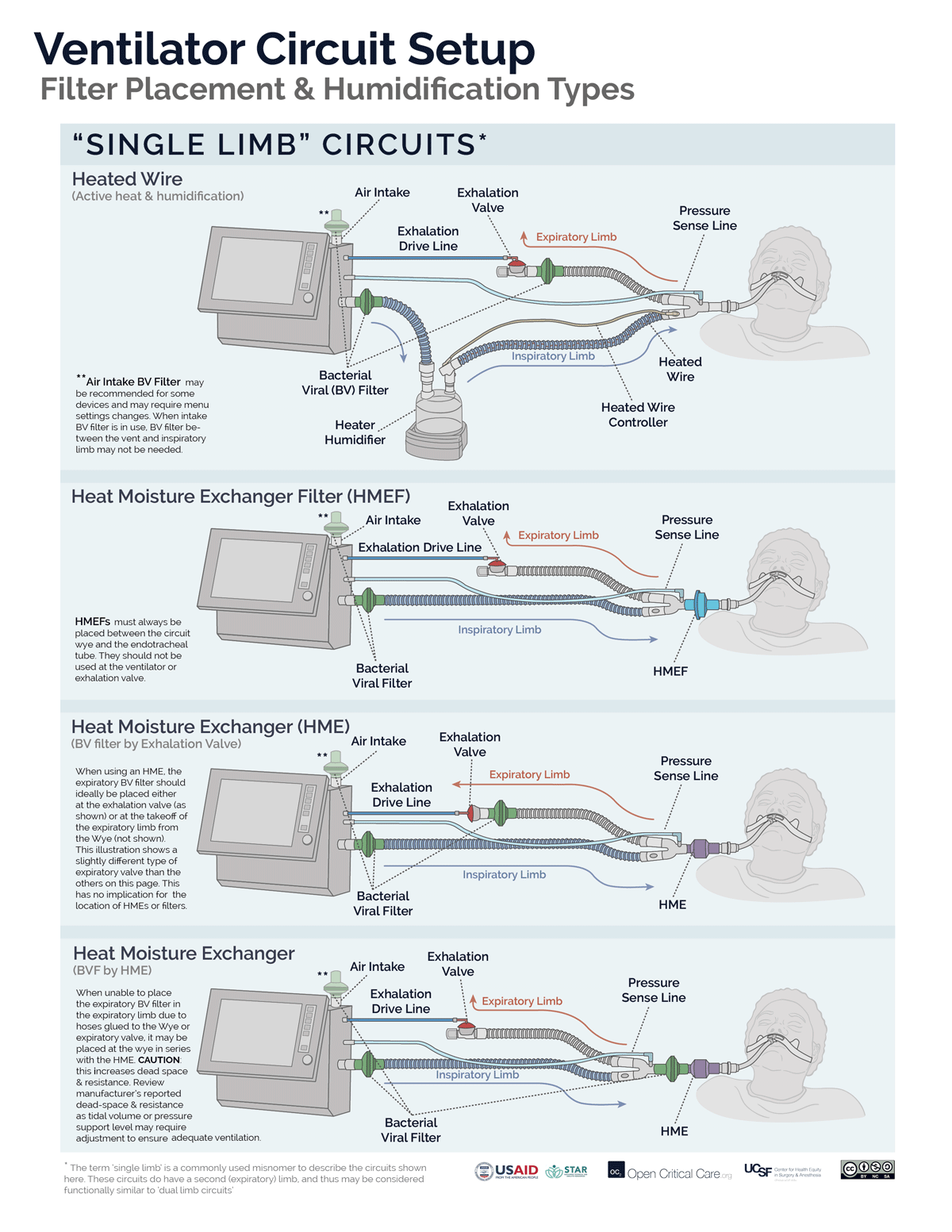
Elimination of a machine mounted inspiratory filter – If a bacterial viral filter is used between the circuit Wye and the patient, then an additional inspiratory filter between the machine and the inspiratory limb may not be necessary to protect the patient (so long as the machine is kept clean and an airway mounted filter and/or expiratory limb filter is used). That is a big “if,” and the use of an inspiratory limb filter at the circuit takeoff is to eliminate this chance of error.
A single inspiratory filter setup (at the wye) has been suggested as an option in settings of severe shortage. This setup may create potential for error and subsequent contamination of the machine. Additionally, the use of one instead of two filters in series significantly decreased viral filtration efficiency. The impact on risk of viral contamination is unknown.
Expiratory limb filter extended use (i.e. not changing between patients) has been suggested by some as an option if severe shortage is faced and appropriate bacterial viral filter is used at the patient. APSF
- Filters may be placed at the air intake, inspiratory limb, patient Wye, expiratory limb and/or exhaust port, however, placement at each of these sites does not provide equivalent function. (Video of filter placement location)
- Ideally a two filter setup should be used (Anesthesia Patient Safety Foundation):
- Inspiratory/Patient filter: the first filter should be placed between the circuit Wye connector and the patient and achieves two things: 1) protects the ventilator and the room from exhaled gases from an infected patient, 2) protects a non-infected patient from a possibly contaminated ventilator. If using an active heat and humidification system, then this should be a bacterial viral filter (not an HME). If not using active heat and humidification, then this should be an HMEF or a bacterial viral filter in series with an HME (HME should be between endotracheal tube and B/V filter). In a dual-limb ICU ventilator, the inspiratory bacterial viral filter may be placed on the inspiratory limb at the takeoff from the ventilator.
- Expiratory filter: A second bacterial viral filter is recommended on the exhalation limb before the exhalation valve, to protect the room environment and healthcare staff from stray particles (and to protect the device in a dual limb circuit setup).
- Placement of filters between the circuit Wye and the patient’s endotracheal tube can add significant deadspace to the circuit, especially for pediatric patients.
Click here to download high resolution version of the images below
Moisture present in patients’ lungs is rapidly lost at high breathing rates.
When breathing dry air, cilia stop functioning properly (in a matter of hours – Hirsch et al J Appl Physio 1975). When the moisture level becomes low, mucous in the patient’s lungs can become thick and hard, and quickly block the patient’s airways, or the endotracheal tube, stopping airflow.
Additionally, heat is rapidly lost to non-humidified air.